We are an award winning product design consultancy, we design connected products and instruments for pioneering technology companies.
Predictive health wearables: What the hype got wrong
Reading time 7 mins
Key Points
- Predictive health wearables have delivered value in specific, well-defined contexts, but early hype overstated their ability to predict disease.
- Bias, uncertainty, and user psychology have proven to be system-level challenges that better models and sensors alone cannot solve.
- The most effective wearables function as decision support tools, embedded within broader healthcare systems rather than standalone predictors.
- The future of predictive health wearables lies in interdisciplinary, context-aware design that prioritises trust, restraint, and human judgement.
Building predictive health wearables that users trust requires clinical insight, technical rigour, and thoughtful system design. Our interdisciplinary team can help — schedule a free discovery call today.
Ben Mazur
Managing Director
I hope you enjoy reading this post.
If you would like us to develop your next product for you, click here
Predictive health wearables have been positioned as a breakthrough moment for healthcare, with devices that not only track our health but also help us manage it proactively. From real-time monitoring and early warnings of disease to personalised prevention, cost savings and improved patient outcomes, the promise of a digital health revolution was compelling.
Yet, as we explored in our Tech Trends 2026 post, innovation is increasingly shifting away from making models smarter and towards building smarter systems. Predictive health wearables offer a timely case study of why that shift is pivotal.
After more than a decade of development, deployment, and real-world use, the industry has learned important lessons about bias, ethics, human behaviour, and where predictive health technology genuinely delivers value. Understanding these lessons is critical for entrepreneurs, startups and product developers shaping the next generation of health wearables.
Predictive health wearables’ original promise
Early predictive health wearables were marketed as tools that could detect illness before symptoms appeared. Continuous monitoring, combined with machine learning and predictive analytics, was expected to uncover hidden patterns in heart and respiratory rates, sleep patterns, potential tumours, and other biometric data. In practice, however, the term predictive blurred important distinctions:
- Correlation was often framed as causation: For example, a rise in resting heart rate or changes in sleep patterns were sometimes interpreted as early signs of illness, when they could just as easily reflect stress, dehydration, travel, or lifestyle changes as commonplace as moving into a new house.
- Risk signals were presented as future outcomes: A statistical increase in risk, such as a higher likelihood of atrial fibrillation or metabolic issues, was often communicated in ways that felt like a forecast, rather than a probability that might never materialise.
- Probabilities were communicated with an air of certainty: Alerts and insights were frequently delivered without clear confidence ranges or limitations, giving users the impression that predictions were more definitive than the underlying data justified, and compelling them to schedule doctors’ appointments.
This framing helped accelerate adoption and investment, but it also set expectations that the technology was not yet fully equipped to meet.
What did the digital healthcare hype get wrong?
Healthcare Prediction vs. Disease Probability
Most predictive health wearables do not predict specific health events. They identify statistical deviations from a personal baseline or population norm and infer risk. That distinction is crucial. A probabilistic signal without context can:
- Trigger unnecessary anxiety.
- Create false reassurance.
- Undermine trust when predictions don’t materialise.
In healthcare, the cost of a false positive is not just technical or financial: it’s psychological, and sometimes clinical.
AI Bias in Health Wearables
In the context of healthcare AI, bias can be defined as any systematic and/or unfair difference in how predictions are generated for different patient populations that could lead to disparate care delivery. Bias in predictive health wearables is no longer a theoretical concern and has been repeatedly observed in real-world examples. Common issues include:
- Perpetuating racial and/or gender disparities, for example, misdiagnosing skin cancer in patients with darker skin, or underestimating women’s heart disease.
- Inaccurate diagnoses for underrepresented groups due to imbalanced training data.
- Resource misallocation, whereby biased algorithms can misdirect resources, can impact both fairness and efficiency.
- AI tools used for health insurance claims are accused of producing claim denial rates 16 times higher than human reviewers.
- Erosion of patient trust in digital healthcare systems and technology.
While personalisation is often positioned as the solution, it can reinforce bias when baseline assumptions are already skewed. The lesson here is clear: bias cannot be addressed solely at the model level. It must be managed at the system level, through uncertainty handling, validation boundaries, and careful communication.
The Ethics of Always-On Monitoring
Always-on monitoring for healthcare devices refers to continuously tracking device status and performance, even when the device is inactive, enabling real-time alerts and responses. This is naturally an essential feature for health wearables, and was assumed to be inherently beneficial: More data, more insights, more agency and better outcomes. In reality, always-on health tracking raises ethical and practical questions:
- Should a system surface a risk signal if there is no clear action?
- What responsibility does a product have for the emotional or mental impact of alerts?
- How can users meaningfully consent to long-term, continuous surveillance of their bodies?
These questions are no longer hypothetical. For many users, health monitoring devices come with psychobehavioral, physical health, and socio-technological risks. For instance, users who start obsessing over their data, in turn creating anxiety and dependence, lose a certain relationship with their bodies and find it difficult to discern how they actually feel apart from what their device is telling them.
Digital Anxiety and User Fatigue
One of the most overlooked outcomes of predictive health wearables has been user fatigue. Users don’t abandon wearables only because of inaccuracy. They abandon them because:
- Alerts feel intrusive or ambiguous.
- Insights lack actionable guidance.
- Monitoring becomes mentally exhausting.
In health contexts, engagement is not a success metric if it comes at the expense of trust and well-being. Systems that demand constant attention ultimately train users to ignore them.
Where are predictive health wearables most effective?
Despite the challenges, predictive health wearables are not failing. They are succeeding — just in narrower, more specific contexts than originally promised. Areas with proven value include:
- Cardiac rhythm detection, particularly atrial fibrillation screening
- Sleep disorder identification, as a triage rather than a diagnostic tool
- Post-operative and recovery monitoring
- Chronic condition trend tracking, where long-term patterns matter more than single predictions
The common thread is that wearables perform best as decision support tools, embedded within broader healthcare systems, rather than standalone predictors. Clinical-grade biomarkers further reinforce this pattern.
Technologies such as continuous glucose monitoring (CGM) demonstrate how predictive wearables deliver the most value when measurement, interpretation, and intervention are tightly linked. CGM succeeds not because it predicts disease, but because it provides reliable, continuous insight into a well-understood biomarker with clear clinical pathways for action.
A similar pattern can be seen in FemTech (technologies dedicated to women’s healthcare innovation). Cycle tracking and hormonal insight tools have delivered meaningful value not by predicting disease, but by supporting long-term pattern recognition, planning, and user-led decision-making. By combining subjective inputs with physiological data and explicitly embracing uncertainty, femtech platforms demonstrate how predictive health wearables can be effective without over-claiming clinical authority.
Other emerging biomarkers, such as blood pressure and hydration, as well as advanced optical sensing technologies, show significant promise but also highlight the limits of prediction without context. While advanced sensors and dynamic photodetectors improve data quality and device miniaturisation, they do not eliminate uncertainty, bias, or the risk of over-interpretation.
The lesson is consistent: improving sensor fidelity strengthens the foundation, but it does not replace the need for thoughtful system design. As biomarkers become more clinical-grade, the responsibility shifts from simply collecting better data to deciding how, when, and whether that data should influence human decisions.
What these lessons mean for product developers
For product teams and innovators, the evolution of predictive health wearables underscores a broader industry shift: value increasingly lies in how intelligence is applied, rather than in the sophistication of the model.
Smarter systems:
- Know when not to alert.
- Communicate uncertainty clearly.
- Integrate seamlessly into care pathways.
- Respect users’ cognitive and emotional limits.
The future of predictive health wearables is not about predicting more events, but rather about intervening more effectively within a broader, holistic, and context-aware system. As Tom Barry, a clinical intelligence analyst, puts it, “We are about to enter a new era of clinical intelligence. The era of ‘digital’ as a separate activity in healthcare – something you do at a screen – will begin to dissolve. We built the nervous system. Now, in 2026, we’re finally ready to give it a brain.”
Designing the next generation of digital healthcare wearables
As the market matures, several design principles are emerging:
- Predict less, contextualise more: Focus on meaning and action, not raw signals.
- Design for uncertainty: Make confidence levels and limitations visible to users and clinicians.
- Optimise for long-term trust: Avoid short-term engagement tactics that erode credibility.
- Treat silence as a feature: Not every deviation requires a notification.
- Support human judgement: The most effective systems augment decision-making rather than attempting to replace it.
These principles reflect a move away from device-centric thinking towards system-level design.
Predictive wearables demand interdisciplinary design
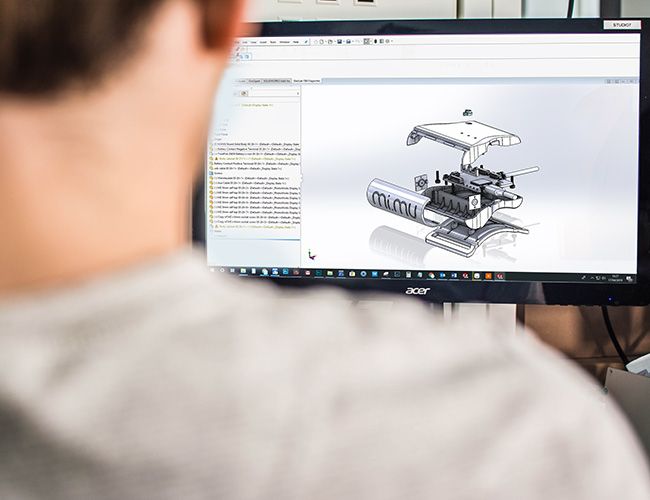
Designing predictive health wearables is an interdisciplinary challenge. Hardware engineers, data scientists, designers, and healthcare professionals are all shaping different parts of the same system. Failures to perform as promised often occur where those perspectives don’t meet.
Predictive systems break down when technical optimisation happens in isolation. Highly accurate sensors are of limited value if their outputs are misinterpreted. Sophisticated models can erode trust if their insights are delivered without clinical or emotional context. Likewise, well-designed interfaces can do harm if they surface signals that lack medical relevance or clear next steps.
The success of devices like the Empatica Embrace, the world’s first FDA-cleared wrist-worn wearable for detecting epileptic seizures, highlights the importance of interdisciplinary collaboration. By combining expertise in neurology, data science, engineering, and product design, the team developed a system that strikes a balance between technical accuracy, clinical validity, and user acceptability. The result was not just a functional device, but one that users were willing and able to trust.
For predictive health wearables, this kind of collaboration is not optional. It is the foundation that allows systems to decide not just what can be detected, but what should be communicated, to whom, and when.
From predictive promises to fulfilled performance
Predictive health wearables are no longer in their experimental phase. They are entering a period of accountability.
The question is no longer whether these devices can collect enough data or run sophisticated models. It is whether they can deliver insight responsibly, equitably, and sustainably within the contextual reality of human variables and complex healthcare systems.
For product developers, this represents an opportunity. Those who embrace restraint, context, and systems thinking will define the next chapter of predictive health wearables, and we’re looking forward to embarking on that journey with them. For a free and confidential consultation with an expert on our interdisciplinary team, schedule a free discovery call today.
Tech Trends 2026: Agentic AI, Edge Intelligence & System Resilience
FemTech: The underestimated healthcare revolution for women
Can the latest medical sensor technologies truly disrupt healthcare?
FAQ’s
What are predictive health wearables?
Predictive health wearables are devices that collect continuous physiological data and use algorithms to identify patterns, trends, or potential health risks. They do not usually predict disease with certainty, but instead indicate probabilities or deviations from a personal baseline. Their primary value lies in supporting earlier awareness and informed decision-making.
How do predictive health wearables work?
Predictive health wearables operate by combining sensor data, such as heart rate, movement, or sleep patterns, with machine learning models. These models look for patterns or anomalies over time, rather than focusing on individual data points. The results are then translated into insights or alerts for users or clinicians.
Why are predictive health wearables not always accurate?
Predictive health wearables rely on probabilistic models rather than direct diagnosis. Accuracy can be affected by sensor limitations, biased training data, and changes in user behaviour or environment. Without sufficient context, predictions may be misleading or incomplete.
What health conditions are predictive health wearables most effective at supporting?
Predictive health wearables are most effective for monitoring cardiac rhythms, screening sleep disorders, tracking recovery, and analysing trends in chronic conditions. These use cases depend on long-term pattern recognition rather than single predictions. They work best when integrated into broader healthcare pathways.
How reliable are predictive health wearables for disease detection?
Predictive health wearables are not designed to diagnose disease. They provide risk signals or early indicators that may prompt further clinical investigation. Reliability improves when results are interpreted by healthcare professionals rather than acted on in isolation.
Why do predictive health wearables cause anxiety for some users?
Predictive health wearables can create anxiety when alerts are frequent, ambiguous, or lack clear next steps. Constant monitoring may lead to hyper-vigilance and over-interpretation of normal bodily variations. This can erode trust and lead to device abandonment.
What is the difference between prediction and probability in health wearables?
Prediction implies a specific future outcome, while probability indicates a likelihood based on available data. Most predictive health wearables operate in the realm of probability, not certainty. Confusing the two has been a major source of misplaced expectations.
How does AI bias affect predictive health wearables?
AI bias can result in less accurate predictions for specific demographic groups. This often results from imbalanced training data or assumptions embedded in system design. Bias affects fairness, safety, and trust in digital healthcare technologies.
Why can't better sensors alone fix predictive health wearables?
Improved sensors enhance data quality but do not solve interpretation or communication challenges. High-fidelity data can still be misused or over-interpreted without proper system design. Thoughtful integration is required to turn better data into better outcomes.
What role do clinical-grade biomarkers play in predictive health wearables?
Clinical-grade biomarkers provide more reliable and meaningful measurements. Their success depends on clear intervention pathways and the ability to provide contextual interpretation. Without these, even high-quality biomarkers can generate confusion rather than clarity.
How does continuous glucose monitoring fit into predictive health wearables?
Continuous glucose monitoring demonstrates how predictive wearables function optimally when measurement, interpretation, and action are closely integrated. It supports real-time decision-making rather than disease prediction. This makes it one of the strongest examples of effective wearable technology.
Why are femtech platforms often more trusted than other predictive wearables?
Femtech platforms tend to focus on long-term pattern recognition and user agency. They openly communicate uncertainty and avoid over-claiming clinical authority. This approach aligns more closely with how biological systems actually behave.
What ethical concerns surround always-on health monitoring?
Always-on monitoring raises questions about consent, psychological impact, and data use. Users may not fully understand the implications of continuous bodily surveillance. Ethical design must consider emotional and cognitive load, not just technical performance.
How do predictive health wearables fit into healthcare systems?
Predictive health wearables are most effective as decision support tools within existing care pathways. They complement clinical judgement rather than replace it. Integration with healthcare professionals improves safety and usefulness.
Why do many users stop using predictive health wearables?
Users often stop using an app because alerts feel intrusive, unclear, or unhelpful. Mental fatigue and loss of trust play a larger role than technical inaccuracy. Long-term adoption depends on restraint and relevance.
What does smarter system design mean for predictive health wearables?
Smarter system design focuses on when to surface insights and when to remain silent. It prioritises context, uncertainty, and human judgement. This approach reduces harm and increases long-term trust.
How can predictive health wearables effectively communicate uncertainty?
They can use ranges, confidence indicators, and clearer explanations of limitations. Avoiding definitive language helps users understand that insights are probabilistic in nature. Better communication reduces anxiety and misinterpretation.
Which disciplines are essential for designing predictive health wearables?
Engineering, data science, design, and healthcare expertise all play critical roles. Failures often occur when these disciplines operate in silos. Interdisciplinary collaboration enables the development of safer and more effective systems.
Why are predictive health wearables moving away from hype-driven claims?
Real-world use has exposed the limits of prediction without context. Regulatory scrutiny, user fatigue, and ethical concerns have prompted a more responsible approach. The focus is shifting from novelty to accountability.
When will predictive health wearables reach their full potential?
Predictive health wearables will reach their full potential as system-level design matures. This includes better integration into healthcare, clearer communication, and stronger interdisciplinary collaboration. Progress depends as much on responsibility as on technology.
Get a quote now
Ready to discuss your challenge and find out how we can help? Our rapid, all-in-one solution is here to help with all of your electronic design, software and mechanical design challenges. Get in touch with us now for a free quotation.
Comments
Get the print version
Download a PDF version of our article for easier offline reading and sharing with coworkers.


0 Comments